



1. Breast cancer an introduction
2. What is Cancer a general introduction
5. Treatments for breast cancer
Breast cancer is the most common type of cancer in women in the United States (excluding cancers of the skin). More than 207,000 new cases will be diagnosed in 2010, and almost 40,000 deaths will result. A woman with average risk factors has about a 1 in 8 chance of developing breast cancer in her lifetime. About 85% of breast cancers begin in the mammary ducts (the tubes that carry milk to the nipples), while the remaining 15% originate in the lobules (the glands that make milk). Breast cancer can occur in both women and men, although male breast cancer is rare (about 1% of all breast cancers). Tumors in the breast tend to grow slowly, with some tumors growing for 10 years before they can be large enough to be palpable. However, other tumors are more aggressive and can grow much more rapidly. Many factors are linked to breast cancer risk, with some factors affecting risk to a greater amount than others. Many risk factors have still yet to be determined and others are not able to be controlled (such as age or family history of breast cancer). Breast cancer is often first suspected when a lump is detected during a self-examination or when an abnormal area is seen on a mammogram. Follow-up tests are necessary to determine if the area is cancerous. Two basic types of surgery to remove breast cancer are available: lumpectomy, in which the tumor and some surrounding tissue are removed, but the rest of the breast is left intact, and mastectomy, where the entire breast is removed. Radiation therapy is almost always warranted following a lumpectomy and can be also used following a mastectomy. A number of chemo and biological therapies are available as treatment for breast cancer which, in combination with early detection, have resulted in a decrease in the number of breast cancer-related deaths over the past 20 years. There are currently over two million breast cancer survivors in the United States. Most survivors lead long and fulfilling lives.
The breast is made up of a complex network of milk-producing sacs (lobes), passageways for carrying milk (ducts), supporting tissue, lymph nodes, glands, muscles and fat. Structure and function of the breasts change during various stages of life, especially throughout puberty and menopause. Each breast has 15 to 20 lobes, which have many smaller sections called lobules. Lobules end in dozens of tiny bulbs that can produce milk. The lobes, lobules, and bulbs are linked by thin tubes called ducts.
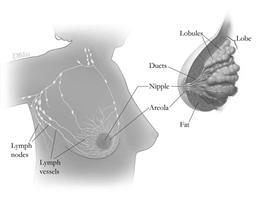
Anatomy of the breast, showing lymph nodes and lymph vessels.
Each breast also has blood vessels and lymph vessels. The lymph vessels are thin-walled, valved structures that carry a fluid called lymph. Lymph fluid carries a variety of substances (including proteins, fats, bacteria and metastatic cancer cells) through the body to the lymph nodes via the lymph vessels. Lymph nodes are small, bean-shaped structures that are found throughout the body. The lymph nodes act to filter substances in the lymph and help fight infection and disease. Clusters of lymph nodes are found near the breast in the axilla (under the arm), above the collarbone, and in the chest.
Normal cells in the body grow and divide to form new cells which are used as the body needs them to replace old cells when they die. These new cells can make up tissues which are the foundation of the organs of the body. Sometimes, old cells don't die as they should but continue to grow, even though the body doesn't need them. When this occurs, these cells can form a mass which is referred to as a tumor. Tumors can be benign (which generally are not a threat to the person) or can be malignant (which can be a threat to life). Cancer results from the growth of a malignant tumor.
Cancer is not one, but a class of diseases in which a cell or group of cells acquire certain genetic affects the function of the organ in which the tumor grows. Once a tumor grows beyond its normal limits, it may invade nearby tissues and organs and affect their normal functions as well. Finally, tumor cells may break off from the original tumor and spread to other parts of the body through the blood vessels. These cancerous cells may then attach to other organs far from the original tumor and grow to form new tumors that can damage those organs. These three steps (uncontrolled growth, invasion, and metastases) differentiate cancerous tumors from benign ones. While most cancers form tumors, some, like leukemia, do not.
Cancer can affect people at all ages. However, the risk for most cancer types increases with age. Generally, about 15% of all human deaths are caused by cancer, with some cancers causing more deaths than others. In the US, cancer is responsible for 25% of all deaths. The most commonly occurring cancer in men is prostate cancer (about 25% of new cases), while in women nit is breast cancer (also about 25%). In the developed world, one in three people will develop cancer in their lifetime.
Cancers are primarily an environmental disease. It is estimated that 90-95% of cases are due to lifestyle and environmental factors (including tobacco usage, diet and obesity, infections, stress and pollutants), while 5-10% are due to genetics. Environmental factors cause abnormalities in the genetic material of the cells and can result in the formation of a cancerous cell.
A variety of options are available for cancer management. These include: chemotherapy, radiation therapy, surgery, as well as some newer regimens, including immunotherapy and monoclonal antibody therapy. Experimental state-of-the-art cancer treatments are also under development . Given the fact that cancer is a generic term for a class of diseases, it is unlikely that any single therapy will result in a cure for all cancers.
Since declaring a war on cancer by President Richard Nixon in 1971, the US alone has spent more than $200 billion to understand disease processes and possible therapies. However, between 1950 and 2005, there has been only a five percent decrease in the cancer death rate. Changes in lifestyles along with novel therapies and technologies will be required if there is to be a substantial reduction in the incidence and reduction of deaths due to cancer.
The following stages describe the extent of the cancer within or external to the breast. Staging is critical to help the physician choose the best treatment regimen for the patient. The stage is based on the size of the cancer, whether the cancer has invaded nearby tissues, and whether the cancer has spread to other parts of the body. Staging may include blood tests, bone scans, CT scans and lymph nose biopsies.
The following are the stages of breast cancer:
Stage 0: Abnormal cells that are nor invasive cancer. These abnormal cells are localized to the lining of the breast duct and have not left that region to invade nearby breast tissue or spread outside the breast duct. Treatment is generally breast-sparing surgery with radiation, although some women chose a total mastectomy.
Stage 1: Early stage invasive breast cancer. Cancer cells have spread to nearby breast tissue, but have not spread beyond the breast. At this stage, the tumor is no larger than three quarters of an inch across.
Stage 2: Is defined as one of the following:
a. The cancer has spread to one of the lymph nodes under the arm and is no more than three quarters of an inch across;
b. The cancer has not spread to the lymph nodes under the arm tumor and is between three-quarters of an inch to 2 inches in size;
c. The cancer has spread to the lymph nodes under the arm and is between three-quarters of an inch to 2 inches across;
d. The cancer has not spread to the lymph nodes under the arm and is larger than 2 inches
Women with Stage 1 or II breast cancer commonly choose breast-sparing surgery followed by radiation. Some women elect to have a mastectomy. Women with Stage II breast cancer often have lymph nodes under the arm removed.
Stage 3: Is locally advanced cancer. Stage 3 cancer is divided into Stage IIIA, IIIB, and IIIC
Stage IIIA is one of the following:
a. The cancer has spread to the underarm lymph nodes that are attached to each other or to other structures, or else the cancer may have spread to lymph nodes behind the breastbone. At this stage, the tumor is no more than 2 inches across
b. The cancer has spread to the underarm lymph nodes that are either alone or attached to each other or to other structures, or the cancer may have spread to lymph nodes behind the breastbone. The tumor is more than 2 inches across
Stage IIIB is a tumor of any size that has grown into the chest wall or the skin of the breast. It is divided into one of the following:
a. The cancer may have spread to lymph nodes under the arm
b. The cancer may have spread to the underarm lymph nodes that are attached to each other or other structures, or else the cancer may have spread to lymph nodes behind the breastbone
c. Inflammatory breast cancer is a rare type of breast cancer. The breast is red and swollen because cancer cells block the lymph vessels in the skin of the breast
Stage IIIC is a tumor of any size that has spread in one of the following ways:
a. The cancer has spread to the lymph nodes behind the breastbone and under the arm
b. The cancer has spread to the lymph nodes above or below the collarbone
The extent to which the cancer has spread, particularly to the number of lymph nodes, or if the tumor in the breast is large, determines whether radiation is used following a mastectomy. Generally, if cancer cells are found in more than 3 lymph nodes under the arm, then radiation is given. Some women have chemotherapy before surgery (neoadjuvant therapy) or after surgery (adjuvant surgery). Administering chemotherapy before surgery can shrink the tumor so that breast-sparing surgery may be performed, while giving therapies after surgery (such as chemotherapy, radiation, hormone or targeted therapies, or combinations of these, can kill cancer cells that remain in the body and therefore can prevent or delay the cancer from coming back.
Stage IV: Is distant metastatic cancer. The cancer has spread to other parts of the body, such as the bones or liver. Treatment of Stage IV cancer is usually chemotherapy, hormone or targeted therapies, or combinations. Radiation may be given to treat defined cancers in certain parts of the body. These treatments generally do not cure the cancer, but may extend life spans.
Recurrent Cancer: Cancer that has returned after a periods of time after it had not been detected. Even when the cancer seems to be completely destroyed, it sometimes can return because undetected cancer cells remained somewhere in the body after treatment. It may return in the breast or other parts of the body, such as the bones, liver, lungs, or brain. Treatment of recurrent cancer is determined by where in the body the cancer has returned.
Cancers occur when a number of different factors interact to produce a malignancy. These include genetic, environmental, medical and lifestyles factors. Knowledge of cancer genetics has vastly improved our understanding of cancer biology and can identify individuals who are at risk for developing the disease. It has also helped to characterize malignancies at the molecular level, which in turn has led to the development of new and more effective treatments. The continually expanding knowledge base of cancer genetics has implications for other aspects of cancer management as well, including prevention and screening for the disease.
What are genes?
Every cell in the body contains genetic material called genes. Each gene is made of a unique sequence of DNA. It is estimated that there are 30,000 genes in each cell. Genes are located on one of the 46 chromosomes in the cell, and are the blueprints which determine the physical characteristics of the person (such as eye color and height). They also control how a cell functions, including how quickly it grows, how often it divides, and how long it lives. To control these functions, genes produce proteins that perform specific tasks in the cell. It is essential that each gene have the correct instructions for making its protein so that the protein can function properly in the cell. Sometimes genes do not work like they should. This is due to an error in the gene, called a mutation. Mutations may be inherited or spontaneous. Inherited mutations are those that a person is born with (a defective gene from one or both parents passed on at birth). Spontaneous mutations are those that can occur in a single cell during the course of a lifetime. They may be caused by exposure to environmental toxins such as radiation or chemicals, changes inside the body, or lifestyle. Cancers occur when a buildup of mutations in genes that control cell growth and division or the repair of damaged DNA do not function properly and allow cells to grow and divide uncontrollably to form a tumor.
Genes and breast cancer:
Most cases of breast cancer (about 90%), are not inherited. These cancers are associated with gene mutations that occur only in breast cancer cells (spontaneous, or somatic mutations) and occur during a person's lifetime.
Hereditary breast cancer accounts for the remaining 10%. This type of cancer is associated with inherited mutations in specific genes. Two genes have been identified so far that are passed from generation to generation with mutations that are important in developing breast cancer. These genes are called BRCA1 and BRCA2. It is important to remember that women inherit an increased risk of cancer, not the disease itself. Therefore, not all women who inherit mutations in genes will develop the disease. Women who are screened through genetic testing and test negative for mutations in the BRAC genes are not without risk for breast cancer, as the majority of breast cancer is caused by spontaneous(somatic) gene mutations.
Breast cancer-related genes:
Mutations in different genes increase the risk of developing breast cancer. These genes include:
BRCA1, BRCA2, CDH1, PTEN, and TP53 genes
BRCA1 (Breast Cancer 1): is a human tumor suppressor gene which produces a protein called breast cancer type 1 susceptibility protein. A tumor suppressor gene is a gene that protects a cell from one step on the path to cancer. BRCA1 functions in breast cells and cells of other tissue. The protein made by the gene helps repair damaged DNA, or else destroys cells if the damaged DNA cannot be repaired. Mutations in the BRCA1 gene can lead to a defective protein being made that does not work properly. When this happens. the damaged DNA is not repaired properly and the cell may grow out of control and lead to formation of a tumor.
Hundreds of mutations have been identified in the BRCA1 gene. While certain mutations are associated with an increased risk of breast cancer, some mutations are in areas of the gene which do not produce a defective protein and therefore do not increase a woman's risk of developing the disease . Women who have an abnormal BRCA1 gene have up to a 60% risk of developing breast cancer.
BRCA2 (Breast Cancer 2): Like the BRCA1 gene, BRCA2 is a tumor suppressor gene that produces a protein called breast cancer 2 susceptibility protein. Although the structures of the BRCA1 and BRCA2 genes are very different, some of the protein's functions are similar. The BRCA2 protein is important for repairing damaged DNA, and a defective BRCA2 protein cannot properly repair the damaged DNA. As a result, mutations that arise in the damage DNA build up. This can cause cells to grow in an uncontrolled way and eventually form a tumor. Hundreds of mutations have been identified in the BRCA2 gene and certain mutations increase a woman's risk of developing breast cancer.
Mutations in the BRCA genes have been linked to other cancers (for example, ovarian and pancreatic cancers).
CDH1: The CDH1 gene, like the BRCA genes, is a tumor suppressor gene. It provides instructions for making a protein called epithelial cadherin or E-cadherin. Cadherins are a group of proteins located on the surface of cells that help neighboring cells stick to one another (a process called cell adhesion). These proteins bind cells together to form organized tissues.
As a tumor suppressor gene, CDH1 is thought to prevent cells from growing and dividing in an uncontrolled manner. Because this protein helps cells stick together, it may also keep cancer cells from detaching from a tumor, traveling through the bloodstream, and invading other tissues (called metastasizing). Abnormal functioning, or the loss of the protein due to mutations in the CDH1 gene may make it easier for cancer cells to detach from a primary tumor and therefore contribute to progression of cancer by increasing proliferation (an increase in the number of cells as a result of cell growth and cell division), invasion and/or metastasis. Mutations in CDH1 are correlated with a number of different cancers, including breast, stomach, colorectal, thyroid, and ovarian cancers. Over 50 mutations have been identified so far in the CDH1 gene.
PTEN: This gene encodes (provides instructions) a protein called phosphatase and tensin homolog (PTEN). PTEN acts as a tumor suppressor gene by acting as part of a chemical pathway that signals cells to stop dividing and causes cells to undergo a process called apoptosis (cell death). These functions prevent uncontrolled cell growth that can lead to the formation of tumors. Mutations in this gene are a step in the development of a large number of cancers. There is also evidence that the protein made by the PTEN gene may play a role in cell movement (migration) and sticking (adhesion) of cells to surrounding tissues.
TP53: The TP53 gene encodes a protein called tumor protein p53. This protein acts as a tumor suppressor. It regulates cell division by keeping cells from growing and dividing too fast or in an uncontrolled manner.
Tumor protein p53 binds to the DNA in the nucleus of the cell. This protein plays a critical role in determining whether DNA that has been damaged by any number of different processes will be repaired or the damaged cell will undergo apoptosis if the DNA cannot be fixed. This prevents cells with damaged DNA from dividing, which helps prevent the development of tumors.
Mutations in the TP53 gene occur in between 20 to 40 percent of all breast cancers. These types of cancers are typically not inherited. The mutations lead to the production of a nonfunctional version of the TP53 protein. The defective protein builds up in cells and cannot regulate cell growth and division. Mutations in the TP53 gene are associated with larger breast tumors and more advanced disease. Recurring tumors are also more likely to have mutations in the TP53 gene.
A number of other genes have been identified as being associated with the development of breast cancer. For more information on these genes, please refer to the following links:
There are five types of standard treatment available to patients with breast cancer. These include: Surgery, Chemotherapy, Radiation Therapy, Hormone Therapy, and Targeted Therapy.
Surgery
Most breast cancer patients undergo surgery to remove the cancer from the breast. Some of the lymph nodes under the arm are usually removed as well and inspected under a microscope to see if they contain cancer cells. There are several forms of surgery that can be carried out.
Breast-Conserving Surgeries
This treatment removes the cancer but not the breast. There are two types:
Lumpectomy: Removes the tumor and some normal tissue surrounding the tumor.
Partial mastectomy: Removes part of the breast that contains the cancer and some normal tissue around it.
Types of surgery that remove the breast include:
Total mastectomy: Removes the entire breast that has cancer
Modified radical mastectomy: Removes the entire breast that has cancer, many of the lymph nodes under the arm, the lining over the chest muscles, and sometimes part of the chest wall muscles.
Radical mastectomy: Removes the breast containing the cancer, chest wall muscles under the breast, and all of the lymph nodes under the arm.
Chemotherapy may be given prior to surgery to shrink the tumor. This reduces the amount of tissue that needs to be removed during surgery. Some patients may be given chemotherapy, radiation therapy, or hormone therapy following surgery to kill any remaining cancer cells.
Chemotherapy
Chemotherapy uses drugs to stop the growth of cancer cells. The drugs may directly kill the cells or else prevent the cells from dividing. Chemotherapy can be taken orally (by mouth) or injected into a vein or a muscle. The drugs then enter the bloodstream and reach cancer cells throughout the body. Chemotherapy can also be administered directly into the cerebrospinal fluid ( ), an organ, or a body cavity such as the abdomen. In these instances, the drugs mainly affect cancer cells in those specific regions.
Types of chemotherapy
There are many drugs that are used in chemotherapy to treat breast cancer. Most are given via infusion (injected), but a few are given orally. The way that the drugs work are different for each one used. They also may have different side effects. Drugs are usually given in combination (called combination therapy) since it has been shown that some drugs act more effectively against breast cancer when given with other chemotherapeutic drugs. The type of chemotherapy used and the scheduling of the drug is dependent on the stage and type of the cancer.
Below is a table listing some of the drugs used in chemotherapy regimens or else under investigation:
Afinitor |
Novartis Pharmaceuticals |
everolimus |
Herceptin-resistant and triple-negative breast cancer |
Arimidex |
|
anastrozole |
Post-menapausal women |
Iressa |
|
gefitinib |
being studied for metastatic breast cancer |
Adrucil |
|
fluorouracil |
used to treat any stage of breast cancer |
Adriamycin |
|
doxorubicin |
used to treat early stage or node-positive breast cancer |
Cytoxan |
|
cyclophosphamide |
used to treat many forms of breast cancer |
Xeloda |
|
capecitabine |
used to treat metastatic breast cancer |
Taxol |
|
paclitaxel |
used to treat any stage of breast cancer |
Ixempra |
|
ixabepilone |
used to treat metastatic or locally advanced breast cancer |
Aromasin |
|
exemestane |
used to treat certain types of breast cancer in post-menopausal women |
Faslodex |
|
fulvestrant |
used to treat metastatic breast cancer in post-menopausal women |
Herceptin |
|
trastuzumab |
a monoclonal antibody used to treat cancer cells that produce more than the normal amount of the HER2 protein. HER2 stands for human epidermal growth factor receptor 2, a protein found on cells which promotes the growth of cancer cells. |
Tamoxifin |
|
tamoxifin |
used to treat metastatic breast cancer and breast cancer in certain patients after surgery and radiation therapy |
Many of the drugs listed are also used for other types of cancers.
Radiation Therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are three main types of radiation therapy: External bean radiation therapy uses a machine to deliver radiation directly to the cancer, and Internal radiation therapy uses a radioactive substance that is placed in sealed needles, seeds, wires, or catheters and inserted directly into or near the cancer (brachytherapy). Systemic radioisotope therapy involves infusion or oral ingestion of unsealed radioactive substances as the method to get the therapy into the body. Radiation therapy works by damaging the DNA of cancer cells, causing them to die (a term called apoptosis). Radiation therapy may be used as a curative or adjuvant (additional therapy usually given after surgery) therapy. There are several types of external beam radiation (including conventional external beam radiation, stereotactic radiation, 3-dimensional conformal radiation, and proton therapy). As with chemotherapy, the way the radiation therapy is administered depends on the type and stage of the cancer.
Hormone Therapy
Hormones are chemicals produced by cells or glands in one part of the body that circulate in the bloodstream and send out messages that affect cells in other parts of the body. Most hormones initiate a response by first combining with a receptor on the surface of the cell or else inside the cell. Hormones can cause certain cancers to grow. Hormone therapy removes hormones or blocks their action and stops cancer cells from growing.
Some drugs listed as chemotherapeutic agents are used in hormone therapy regimens. For example, tamoxifen is metabolized in the body into hydroxytamoxifen, which binds to the estrogen receptor on some breast cancer cells. Estrogens are hormones that promote the development of female secondary sexual characteristics, such as the breasts. Some breast cancer cells require estrogen to grow. Tamoxifen binds to the estrogen receptors of these cells and, unlike estrogen, does not activate the receptor and therefore prevents the cancer cell from growing.
Instead of blocking the binding of estrogen to its receptor on breast cancer cells, some drugs decrease the levels of estrogen in the body. An example of these types of drugs are the aromatase inhibitors. Aromatase is an enzyme that synthesizes estrogen. Aromatase inhibitors block the action of the aromatase enzyme and therefore block the synthesis of estrogen. This lowers the amount of estrogen in the body and slows the growth of cancer cells that have estrogen receptors.
Hormone therapies may be used in conjunction with other therapies to produce a more effective treatment regimen.
Targeted Therapy
A subset of chemotherapy that uses drugs or other substances to attack cancer cells without harming normal cells is called targeted therapy. While most chemotherapeutic drugs act in a non-specific manner (that is, they usually attack cancer cells as well as normal cells), targeted therapy is designed to hit specific cancer cells and not normal cells, thereby reducing the number and severity of side effects that usually accompany standard chemotherapy. Because less side effects occur, the amount (dosage) of targeted drugs that can be given to a patient is more effective at killing the cancer cells. A number of different types of targeted therapies exist. Monoclonal antibodies and tyrosine kinase inhibitors are two types of targeted therapies used into treat breast cancer. PARP inhibitors are a type of targeted therapy being studied for use of specific breast cancer types.
Monoclonal antibody therapy uses antibodies that are made in the laboratory. These antibodies can identify substances on cancer cells (tumors-specific antigens: molecules that are present on the surface of cancer cells and not normal cells) or other substances that can help cancer cells grow. The antibodies specifically attach to the antigens or substances and can kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies have been designed to carry drugs, toxins (poisonous substances that can kill the cancer cells), or radioactive material directly to cancer cells. Herceptin (generic name: trastuzumab) is a monoclonal antibody that binds selectively to the human epidermal growth factor protein HER2, which sends growth signals to breast cancer cells. The antibody blocks the effects of HER2, preventing the cancer cells from growing out of control. About one-fourth of patients with breast cancer have tumors that have more than normal amounts (overexpression) of HER2 (overexpression of HER2 is associated with an increase in disease recurrence and a poor prognosis) and may be treated with trastuzumab combined with chemotherapy.
Tyrrosine kinases are enzymes that work in a number of processes and are responsible for carrying out key events in the body. One of these events is cell growth. Some defective tyrosine kinases have been associated with causing or maintaining cancers. Drugs that can specifically target a defective tyrosine kinase and block the signals needed for the tumor to grow can be instrumental in controlling the growth of the cancer cells. Lapatinib is an example of a tyrosine kinase inhibitor. It is an orally active drug given for breast cancer and other solid tumors. Lapatinib inhibits the tyrosine kinase activity of HER2 as well as EGFR (epidermal growth factor receptor), thereby preventing the growth signals produced by these two proteins to support uncontrolled growth of the cancer cells. Tyrosine kinase inhibitors may be used in combination with other anticancer drugs.
PARP inhibitors are a type of targeted therapy that block DNA repair. PARP1 is an enzyme that is important in repairing breaks in DNA. Several forms of cancer are more dependent on PARP1 than are normal cells, thereby making PARP1 an attractive target for therapy. By inhibiting the DNA repair function of PARP1, DNA that contains breaks cannot be repaired and therefore PARP inhibitors may cause cancer cells to die. Examples of PARP inhibitors in clinical trials include: Iniparib (particularly for triple-negative breast cancer, which is a breast cancer whose cells do not contain the estrogen receptor, progesterone receptor, and HER2. This breast cancer subtype is more aggressive and less responsive to standard treatment and has a poor prognosis); Olaparib, which acts against cancers with hereditary BRAC1 or BRAC2 mutations. BRAC1 and BRAC2 are called tumor suppressor genes (genes that protect cells from one step on the path to cancer. When a tumor suppressor gene is mutated and no longer functions normally, the cell can progress to cancer, usually in combination with other genetic changes). Patients with BRAC1/BRAC2 mutations may be predisposed to certain forms of cancer; Veliparib, which targets PARP1 and PARP2. PARP inhibitors may be used in combination with other chemotherapeutic agents to increase their efficiency in combating breast cancer.